If you are affected by dry or watery eyes a dedicated specialist evaluation in a dedicated clinic is available. Effective treatment plans now offer help to the vast majority of dry/watery eye patients. ADP-EyeCare practitioners are always looking for steps forward in the examinations and care for patients, so not every test, exam, treatment, therapy or product is delivered in the same way by every practitioner at the same time, there is a constant process to evaluate and seek to improve already excellent results.
Burning, stinging, grittiness, itching, soreness, tired eyes – these may be Dry Eye symptoms


Common symptoms can include:
|
What are the symptoms?
The symptoms can be varied in nature and degree, they can occur more in some environments and when doing certain tasks, and interestingly many patients don’t relate these symptoms to dryness. Sometimes these symptoms only occur, or are worse in warm, dry, air conditioned environments, in the office or on aircraft. Certain tasks such as reading, using a computer or driving can also exacerbate the problems. If this sounds familiar help is almost certainly available.
What is causing the symptoms?
There is more than one form of dry/watery eye; there may be an insufficiency of quantity of tears, a reduction in the quality of tears or a combination of both. Recent research has shown the quality of tears to be the most common factor.
Factors that influence your tears
 Influences can be:
Influences can be:
- Disease such as Rheumatoid Arthritis and diabetes
- Hormonal imbalances
- Skin conditions
- Medications
- Increasing age
- Eye/lid infection/inflammation
Many patients have tried, without success, to address their dry/watery Eye symptoms for many years. Probably trying some of the many drops, either prescribed or off the shelf. In many cases these have given little or no relief.
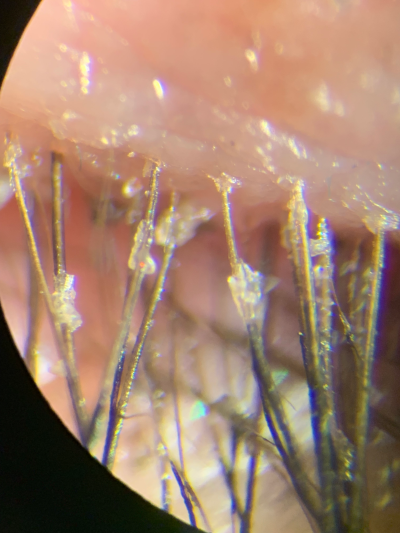
Here is a real life example of a a successful treatment for a lid condition, the patient, a contact lens wearer, had found lenses becoming increasing uncomfortable over years, even having to attend an eye hospital while abroad, trying many different dry eye drops or having new lenses prescribed didn't help. Below are images taken before and after specific treatment that not only resolved the lid appearance but solved the contact lens discomfort problems as well.
 |
 |
| superior lid and lashes 16 March 2019 |
superior lid and lashes, 13 April 2019 |
How can we help?
Please express your interest in a Dry Eye Assessment by email (please see specific regions below), so an appointment can be structered to help you best, include your symptoms and previous eye care both self-treatments and professional. These Dry Eye Clinic appointments are not funded by the NHS so a private fee will be payable, you will be advised of that before making the appointment. a detailed assessment of your dry/watery eye, may include some of, if not more than, the following steps:
- Health and medication history
- Symptoms/Past dry/watery eye treatments
- Tear quantity/quality assessments
- Microscope examination of the front of the eye and lids
- Scanning/imaging of your eye and lids
- At end of the Dry Eye Assessment the findings will be discussed and a treatment plan recommended. You may be offered in-practice treatments and/or instructed you fully on how to obtain the best benefit on use of treatments you can do at home, then a follow-up visit to monitor progress will be arranged.
What do I do next?
If you would like to contact us for non-urgent eye care discussions related to dry eyes or contact lenses you can by email:
- Andrew D Price (Nantwich, Glossop, Widnes or general enquiries)
This email address is being protected from spambots. You need JavaScript enabled to view it. - Elizabeth Ralph (East Midlands and South Yorkshire)
This email address is being protected from spambots. You need JavaScript enabled to view it. - Vanessa Uden (Surrey, Hants, Berks)
This email address is being protected from spambots. You need JavaScript enabled to view it. - Mr Ganeshbabu Mahalingam (West Yorkshire)
This email address is being protected from spambots. You need JavaScript enabled to view it. - Mr Mohamed Ayyaz Kasmani BSc(Hons) MCOptom (West London)
This email address is being protected from spambots. You need JavaScript enabled to view it. - Mr Colin Jones FBDO(Hons) CL (Widnes)
This email address is being protected from spambots. You need JavaScript enabled to view it.
Personal portfolios can be found here:



