 ADP-EyeCare professionals prescribe a large range of contact lenses (legally they are medically devices so only registered Contact Lens Opticians, optometrists and doctors are allowed to do this). They also provide first-class aftercare services to support your successful wear. Many lens options are available, which can be a little bewildering, they will give you expert guidance.
ADP-EyeCare professionals prescribe a large range of contact lenses (legally they are medically devices so only registered Contact Lens Opticians, optometrists and doctors are allowed to do this). They also provide first-class aftercare services to support your successful wear. Many lens options are available, which can be a little bewildering, they will give you expert guidance.
They may hold specialist qualifications in contact lens practice and teach other practitioners on the subjects of contact lenses and dry eye, the aim is always to find the lens type that suits your lifestyle and gives you the best possible vision and comfort. Every eye is unique, they use exams and tests to identify pre-existing conditions that all too often are the cause of lens wear not being successful – if you have stopped contact lens wear in the past, as many do, it could well be these conditions, which can be improved, were missed.
If you have been told you are not suitable for contact lenses a second opinion could be worthwhile. They particularly welcome the more interesting cases: astigmatism; multifocal; post-ocular surgery; post-LASIK; myopia control, etc.
They like to think they are always looking for steps forward in examinations and care for patients, so not every test, exam, treatment, therapy or product is delivered in the same way by every practitioner at the same time, as they evaluate and constantly look to improve the already excellent results.
Are they for me?
Some people want to wear lenses occasionally, for socialising or sports, while others want to wear them all the time because they may get better vision, for convenience or just to have a different look.
The advances in contact lens materials and designs in recent years have led to
- Improved quality of vision
- Ease of use and handling
- More comfortable wear
- A wider range of prescriptions
Many people who thought, or have been told, that they were unsuitable for contact lenses may now have this option open to them.
ADP-EyeCare practitioners may choose not prescribe lenses to be slept in – studies have shown the risk of serious eye infections is six times higher with these lenses. They like to provide full contact lens care for their patients, so do not prescribe or provide after-care related to lenses obtained other than from the practice itself. The supply of lenses is legally restricted, rather like medicines, for good reasons, some companies providing lenses choose not to observe the letter, or even the spirit, of the law and provide ‘substitutes’ or even fake labelled lenses. Your eyes, and your practitioner's ability to sleep well, is too precious to take these risks!
Prescribed contact lenses and given up before?
ADP-EyeCare practitioners especially welcome patients who have dropped out of contact lens wear previously. They belive every eye is unique, they use exams and tests to identify pre-existing conditions that all too often are the cause of lens wear not being successful – if you have stopped contact lens wear in the past, as many do, it could well be these conditions that can be improved were missed.
What are the symptoms?
The symptoms causing patients to stop contact lens wear can be varied in nature and degree, they can occur more in some environments and when doing certain tasks.
Common contact lens symptoms can include:
|
 |
Sometimes these symptoms only occur, or are worse in warm, dry, air conditioned environments, in the office or on aircraft. Certain tasks such as reading, using a computer or driving can also exacerbate the problems. If this sounds familiar ADP-EyeCare practitioners can almost certainly help.
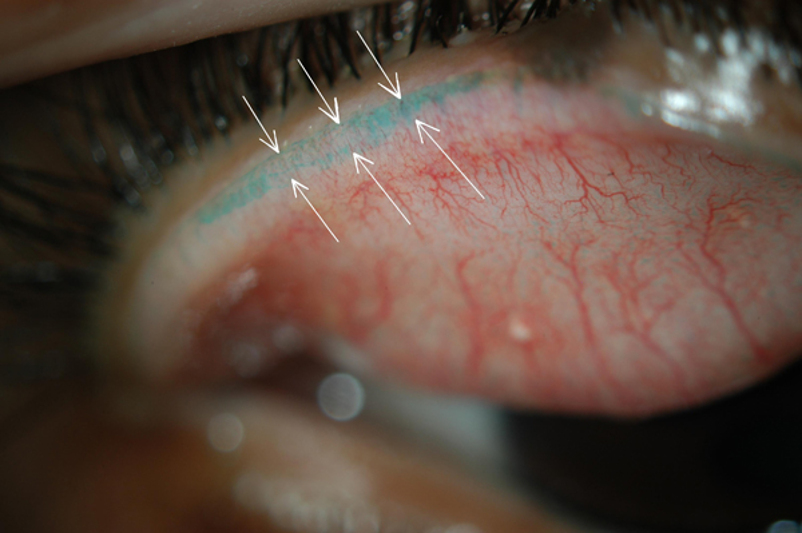
What is causing the symptoms?
The eye’s surface and lids need to be at an optimum for successful contact les wear, in many patients it isn’t; there may be an insufficiency of quantity of tears, a reduction in the quality of tears or a combination of both. Recent research has shown the quality of tears to be the most common factor. The good news is once the specific problem is identified simple treatments can help in the vast majority of cases. For these people replacing one type of lens with another, without identifying the underlying cause rarely helps significantly.
How am I prescribed contact lenses?
 A starting point is a recent ‘general eye exam’ or ‘sight-test’ and then as Eye Care Professionals who like to specialise in contact lenes they will see you for a consultation. Unless you are currently wearing contact lenses it may be preferable to evaluate your contact lens wear first. They will carry out a detailed examination. Before your appointment you may complete a clinical questionnaire. The various lens options that are appropriate to you will be discussed and the surface of your eye and lids examined and test your tears. Next an in-depth discussion on how best to proceed. If you wish, provided you are suitable, an order will be placed for initial assessment lenses.
A starting point is a recent ‘general eye exam’ or ‘sight-test’ and then as Eye Care Professionals who like to specialise in contact lenes they will see you for a consultation. Unless you are currently wearing contact lenses it may be preferable to evaluate your contact lens wear first. They will carry out a detailed examination. Before your appointment you may complete a clinical questionnaire. The various lens options that are appropriate to you will be discussed and the surface of your eye and lids examined and test your tears. Next an in-depth discussion on how best to proceed. If you wish, provided you are suitable, an order will be placed for initial assessment lenses.
At your next appointment you will be assessed wearing the lenses and again reviewed around a week later – at this point if all is well they will then place an order for further lenses.
You will be taught on how to place and remove your lenses. You will be shown how to care for them, what to do and what not to do. Once they are confident in your ability to handle your lenses correctly you will be able to take them away. Most patients are successful at this first ‘teaching’ appointment, but don’t worry if you are not – you will be given as many appointments as you need to achieve this.
What type of lenses?
 Contact lenses are now available in soft, rigid and hybrid materials. They can be made to single vision or multifocal prescriptions and can correct astigmatism. There are pros and cons to every design and these will be explained to you once you have been examined and discussed your needs known.
Contact lenses are now available in soft, rigid and hybrid materials. They can be made to single vision or multifocal prescriptions and can correct astigmatism. There are pros and cons to every design and these will be explained to you once you have been examined and discussed your needs known.
Regular lens replacement has proven to be the healthiest way to wear lenses that are changed daily, fortnightly or monthly. Rigid lenses should be changed at around twelve months.
What are the charges?
Because there are so many designs, care products and frequency of replacement it is not possible to provide accurate charges in general information such as this. They will be able to give you some indication as more is known about your interest in specific lenses and past eye history, it may be possible to give you some approximate ideas by email and then specific charges at an appointment.
What do I do next?
If you would like to contact us for non-urgent eye care discussions related to dry eyes or contact lenses you can by email:
- Andrew D Price (Nantwich, Widnes, Glossop or general enquiries)
This email address is being protected from spambots. You need JavaScript enabled to view it. - Elizabeth Ralph (East Midlands and South Yorkshire)
This email address is being protected from spambots. You need JavaScript enabled to view it. - Vanessa Uden (Surrey, Hants, Berks)
This email address is being protected from spambots. You need JavaScript enabled to view it. - Mr Ganeshbabu Mahalingam (West Yorkshire)
This email address is being protected from spambots. You need JavaScript enabled to view it. - Mr Mohamed Ayyaz Kasmani BSc(Hons) MCOptom (West London)
This email address is being protected from spambots. You need JavaScript enabled to view it. - Mr Colin Jones FBDO(Hons) CL (Widnes)
This email address is being protected from spambots. You need JavaScript enabled to view it.
Personal portfolios can be found here: